|
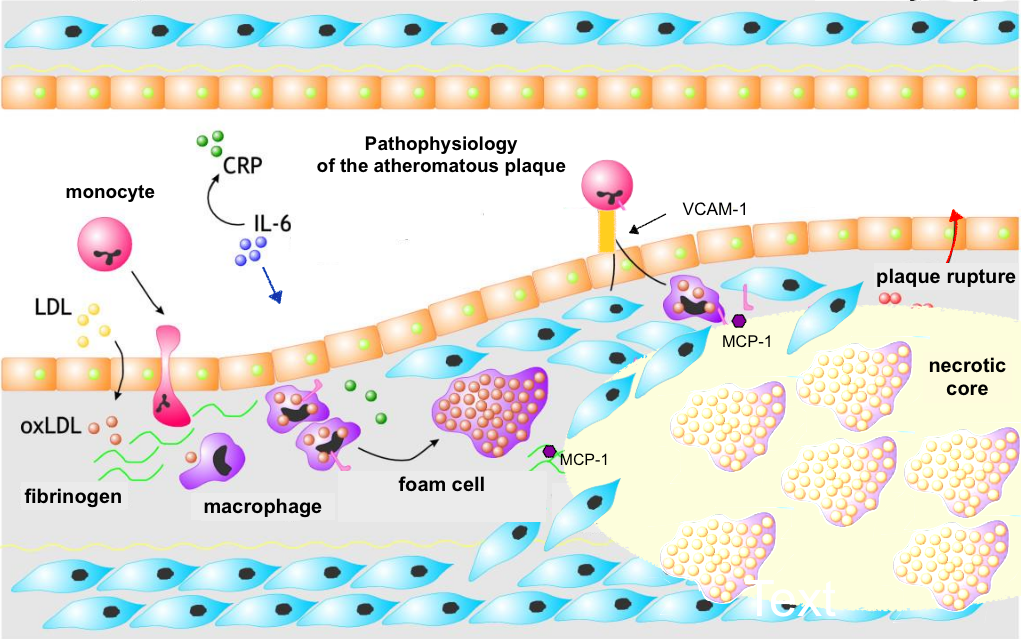
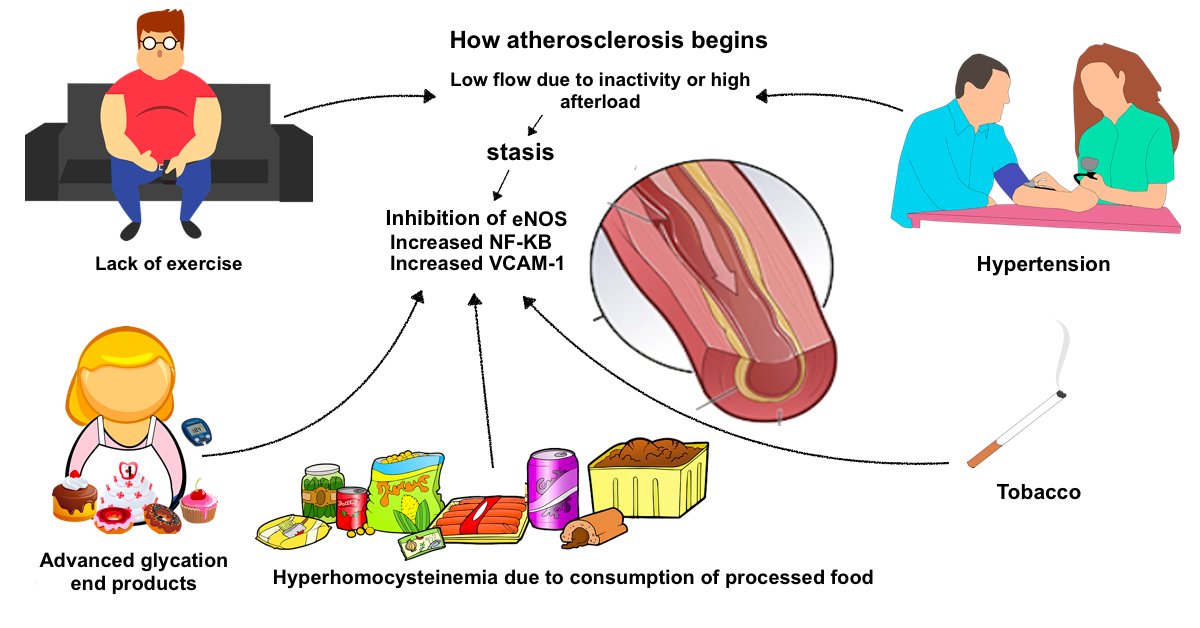
Atherosclerosis begins with an increase in LDL-P levels, that is, an increase in the number of small and dense LDL particles primarily as a result of excess refined carbohydrates (sugar and flour) which stimulate insulin secretion and fructose (juices and sweetened beverages) induced lipogenesis. Smaller LDL particles and VLDL enter the subendothelial space in proportion to their serum level. Apoprotein B of LDL and VLDL interacts with proteoglycans and LDL undergoes oxidation that initiates an inflammatory response. Chronic periodontitis or chronic infections with Chlamydia pneumoniae or Helicobacter pylori activates IL-6 and C-reactive protein and contributes to the inflammatory process. The activation of NF-KB as a signal transducer for atherosclerosis and the inactivation of eNOS (which is the endothelial nitric oxide synthetase that produces nitric oxide) is the result of: -A sedentary lifestyle or hypertension resulting in stasis and decreased shear stress. Atheromatous plaques begin at the bifurcations of the arteries.
-The consumption of refined carbohydrates such as flour and the excesses of fructose from sweetened beverages resulting in an increase in the products of advanced glycation, - Tobacco consumption - The insufficient consumption of fruits and vegetables that results in hyperhomocysteinemia and a deficiency of nitrates and polyphenols in the diet. Inactivation of eNOS results in vasospasm. Activated endothelial cells express monocyte adhesion molecules known as VCAM-1 and chemokine MCP-1. Monocytes bind to VCAM-1 and MCP-1 facilitates the transmigration of monocytes to the subendothelial space. Monocytes are converted into macrophages and express receptors that allow phagocytosis of oxidized LDL cholesterol, VLDL and ApoE residues. The macrophages overflow with lipids and become foam cells. As the space fills with foam cells, they produce chemotactic and proliferative factors that recruit smooth muscle cells that migrate to form a fibrous barrier. If the fibrous layer is firm, the atherosclerotic plaque is stable but at the same time there is less likelihood of regression. If it forms a necrotic center the fibrous layer is more fragile and plaque rupture is more likely .. To see this process in greater detail here is a more extensive summary: Linton MF, Yancy PG, Davies SS, et al. The role of lipids and lipoproteins in atherosclerosis. Endotext
0 Comments
Multiple recent medical research studies have shown that exercise, even just walking for several hours a week, can prolong life, decrease the risk of 13 types of cancer, and even prolong survival time in patients with advanced colon cancer.
A prospective cohort study published in October 2017 in the American Journal of Preventative Medicine followed 62,178 men (mean age 70.7 years) and 77,077 women (mean age 68.9 years) for 13 years. They found that walking between 2 and 7 hours per week decreased mortality by 20% (HR = 0.74 CI 0.72 to 0.76). [1] A prospective cohort study published in BMJ in February 2018 followed 1181 men between 71 and 92 years of age without pre-existing cardiovascular disease for 5 years to determine their level of physical activity. This study showed that even mild physical activity such as gardening or walking the dog, decreased mortality by 17% (HR = 0.83 CI 0.77 to 0.90) and if it accumulates 150 minutes per week the mortality decreases by 41% (HR = 0.59 CI 0.43 to 0.81). [2] In an investigation published in JAMA in June 2016 with 1.44 million participants and an average age of 59 years showed that exercise decreases the probability of contracting 13 of 26 types of cancer: adenocarcinoma of the esophagus (HR, 0.58, 95% CI, 0.37-0.89), liver (HR, 0.73, 95% CI, 0.55-0.98), lung (HR, 0.74, 95% CI, 0.71-0.77), kidney (HR, 0.77, 95% CI, 0.70-0.85 ), gastric (HR, 0.78, 95% CI, 0.64-0.95), endometrial (HR, 0.79, 95% CI, 0.68-0.92), myeloid leukemia (HR, 0.80, 95% CI, 0.70-0.92), myeloma ( HR, 0.83, 95% CI, 0.72-0.95), colon (HR, 0.84, 95% CI, 0.77-0.91), head and neck (HR, 0.85, 95% CI, 0.78-0.93), rectal (HR, 0.87 95% CI, 0.80-0.95), bladder (HR, 0.87, 95% CI, 0.82-0.92), and breast (HR, 0.90, 95% CI, 0.87-0.93). [3] Surprisingly, even patients who already have colon cancer have benefited from walking. In a study conducted by Harvard University of 992 men with stage III colon cancer, it was shown that 30 minutes of exercise per day decrease mortality compared to similar patients, in 42%. [4] How does exercise prolong life, even in cancer patients? It is theorized that because exercise increases glucose metabolism, and therefore decreases the level of circulating glucose in the blood, this results in a decrease in insulin levels and eventually a decrease in obesity. High levels of insulin result in a decrease in insulin-like growth factor binding proteins 1 and 2 (IGFBP1 and IGFBP2), resulting in high levels of insulin-like growth factor-1 (IGF-1.). High levels of IGF-1 increase the risk of cancer of the breast and prostate, but also accelerate cell proliferation. and therefore the growth of several types of tumors with IGF-1 receptors. An increase in exercise and decrease in carbohydrate consumption results in a decrease in insulin and IGF-1 and therefore decreases the proliferation of cancer cells. [5] In summary, in patients with cancer it has been shown that the benefit may come from the decrease in circulating insulin levels, because insulin helps multiply the tumor cells. [6] In addition to decreasing insulin levels, and therefore IGF-1, exercise decreases estrogen levels. [7] References: 1. Patel AV, Hildebrand JS, Leach CR, et al. Walking in relation to mortality in a large prospective cohort of older US adults. Am J Prev Med 2018 Jan;54(1):10-19. 2. Jefferis BJ, Parsons TJ, Sartini C, et al. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: does volume of activity matter more than pattern of accumulation? Br J Sports Med Published Online 12 February 2018. 3. Moore SC, Lee I, Weiderpass E, et al. Association of Leisure-Time Physical Activity With Risk of 26 Types of Cancer in 1.44 Million Adults. JAMA Intern Med. 2016;176(6):816–825. 4. Blarigan EV, Fuchs CS, Niedzwiecki D, et al. American Cancer Society Nutrition and Physical Activity Guidelines after colon cancer diagnosis and disease free, recurrence free, and overall survival in CALGB 89803 J Clin Oncol 35, 2017 (suppl/abstr 10006) 5.Manjinder S. Sandhu, David B. Dunger, Edward L. Giovannucci; Insulin, Insulin-Like Growth Factor-I (IGF-I), IGF Binding Proteins, Their Biologic Interactions, and Colorectal Cancer, JNCI: Journal of the National Cancer Institute, Volume 94, Issue 13, 3 July 2002, Pages 972–980, 6. Brown JC, Rickels MR, Troxel AB, et al. Dose response effects of exercise on insulin among cancer survivors. Endocr Relat Cancer. 2018 Jan;25(1):11-19. 7. Brown JC, Kontos D, Schnall MD, Wu S, Schmitz KH. The Dose–Response Effects of Aerobic Exercise on Body Composition and Breast Tissue among Women at High Risk for Breast Cancer: A Randomized Trial. Cancer prevention research (Philadelphia, Pa). 2016;9(7):581-588. doi:10.1158/1940-6207.CAPR-15-0408. Tinnitus is caused by damage to the sensory hair cells in the cochlea of the inner ear. In the absence of stimuli at a particular frequency it is theorized that there is an imbalance between excitatory and inhibitory neural pathways resulting in neural hyperactivity. There are measures which can help to prevent tinnitus but unfortunately in the vast majority of cases there is no effective treatment. Once it is confirmed that the tympanic membrane is normal and there is no cerumen in the ear canal, no effusion, no infection, and if the tinnitus is persistent and bothersome, the best thing is an audiological examination. Audiograms help to determine the pattern of hearing loss, and to indicate if there is significant risk of tumor, which is an unlikely cause. If there is hearing loss associated with bothersome tinnitus the use of hearing aids is sometimes helpful.
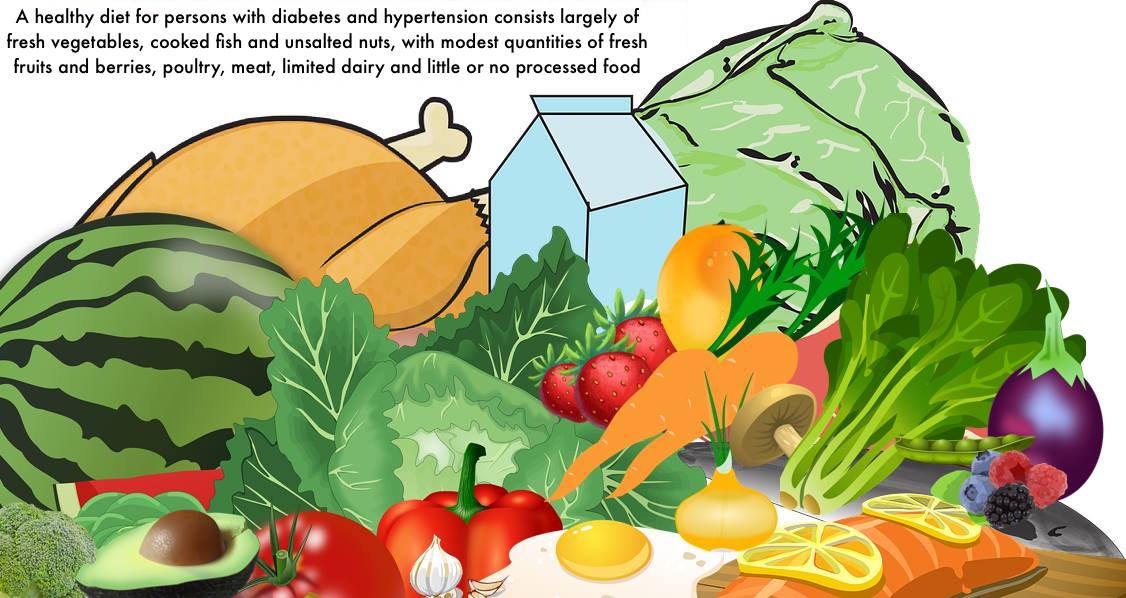
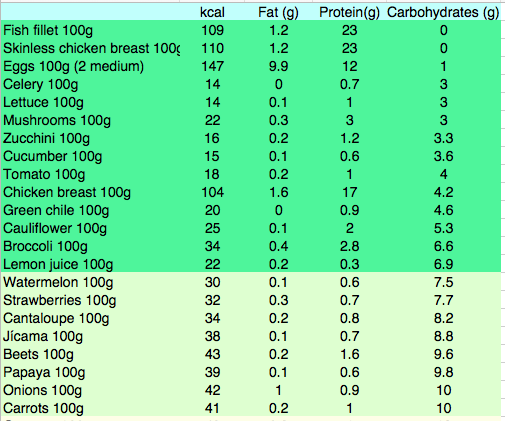
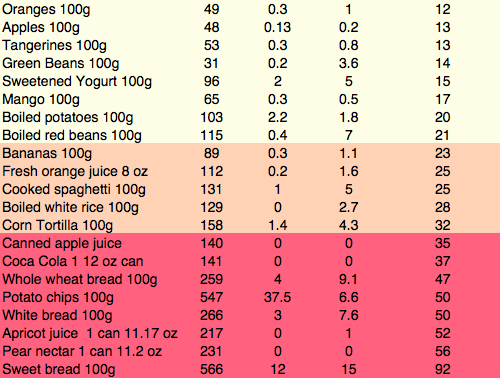
Tinnitus prevention includes: 1- Use NSAIDs infrequently or not at all. 2- Increase routine consumption of dietary fresh fruits, berries, unsalted nuts, fish, herbs and spices in order to obtain sufficient zinc, magnesium, flavonoids and other polyphenols. 3- Do not listen to loud music with headphones or ear buds. 4- Eliminate artificial flavorings and sweeteners, especially aspartame. At a later date we will publish a complete article about the genetics of age related hearing loss and the rationale and details behind specific preventive dietary measures. The New England Journal of Medicine mentions psychotherapy in this review article. The issue of psychotherapy mentioned in this article merits clarification. Tinnitus represents a malfunction of the central nervous system which is exacerbated by the absence of normal auditory stimulation, and may be the first symptom of hearing loss. While hearing loss can be measured there is still no way to measure tinnitus with instruments. People who have very loud and persistent tinnitus may suffer from depression and panic when they realize that it is not improving. Initial management may include sound machines with white noise, rain, waves or other sounds to mask the tinnitus until it becomes less distressing. Eventually after about five years patients may reach a state where the tinnitus is present, but they do not feel emotional distress with it. Until they reach acceptance psychotherapy can be beneficial in some cases. A review article can be found at the following link Rothaus C. What nonpharmacologic approaches presently exist for the management of tinnitus? NEJM Resident 360 Noone has definitively proven the cause of Alzheimer's disease yet, however there are certain things that everyone agrees on. There is a genetic predisposition in some types. The biomarker is the deposition of beta amyloid protein in plaques found on autopsy, and more recently by PET scan, and this deposition is detectable a decade before symptoms begin. However attempts to cure the disease by eliminating beta amyloid protein have been less than successful. What has been shown over the years is that there is a diffuse inflammatory process, perhaps a single common pathway with many causes, which leads to the deposition of beta-amyloid. The heartening finding on epidemiological and retrospective case control studies was the effect of Ibuprofen on disease initiation and progression. These results have not been born out by clinical trials, and many have suggested the failure of clinical trials is due to the need to initiate treatment before symptoms begin. The enthusiasm by researchers for this idea is understandable, even as geriatricians around the world shake their heads. What about the side effects of ibuprofen in the elderly which include gastrointestinal bleeding and renal insufficiency? How do we figure out who these people are that need treatment? This study is a first step in solving the answer to the first question: How to figure out who needs treatment? These researchers report developing an ELISA test on saliva for beta amyloid protein which can detect Alzheimer's disease prior to clinical manifestations. Once that is solved the next question will be what delivery system (perhaps a nasal aerosol?) do we need to bypass the kidneys and GI tract. McGeer PL, Guo JP, Lee M et al. Alzheimer's Disease Can Be Spared by Nonsteroidal Anti-Inflammatory Drugs. J Alzheimer's Dis (2018) 62 (3): 1219-1222 The paradigm for the prevention and cure of early type 2 Diabetes has been shifting away from using pharmaceuticals over the past 10 years and toward the more enduring results which can be achieved by modifying diet and increasing exercise. In the early stages of the disease compliance with increased physical activity and consistent avoidance of starches and foods with high fructose content is generally all that is required in order to stabilize glucose well below 200. The goal is not to increase insulin levels in the body, but to decrease the amount of insulin that the body requires. When food is consumed by the pre-diabetic the beta cells of the pancreas secrete insulin in an amount proportional to the carbohydrate load. Two hours after a high-carbohydrate meal, the high circulating insulin levels may drop blood sugar levels and make one so hungry that the patient resumes eating. Increase of circulating lnsulin levels will increase corporal fat deposition. If fructose is consumed together with glucose this will stimulate simultaneous gluconeogenesis and fatty acid synthesis in the hepatocytes and the fatty acids and triglycerides which are produced may be deposited in the mesenteric distribution leading to central obesity. The greater the level of obesity, the more resistant the patient is to insulin. The pancreas increases insulin secretion even more until eventually the pancreas no longer produces adequate insulin supplies. So we can talk about three phases of type II diabetes The first phase, known as prediabetes, is asymptomatic. The patient eats carbohydrates in excess, secretes a large amount of insulin, gains weight, and circulating glucose levels are still completely normal. One of the findings of the physical examination of this phase is known as acanthosis nigricans, a black discoloration of the neck and armpits caused by high insulin levels. The resistance of the cells to insulin increases gradually as the patient gets fatter, but the pancreas manages to always produce more and more insulin to maintain normoglycemia. The second phase of type II diabetes is slightly symptomatic because although the person still produces insulin, this amount of insulin is not sufficient to keep the glucose level below 180. In this phase the patient is still overweight. Eventually in the third phase of type II diabetes the pancreas reduces insulin production and the person is frankly hyperglycemic. The patient loses weight quickly, because without insulin, glucose can not enter the cells. In this phase it is already too late to cure the disease because since the pancreas does not produce enough insulin the patient begins to look more like type I diabetes. There is a propensity towards malignant external otitis, diabetic retinopathy, renal insufficiency, and ulcerations and gangrene of the feet. To cure the disease it is necessary to attack the problem from all sides while the pancreas still produces insulin. It is a bit like chemotherapy for cancer, which requires sacrifice and determination, because changing the dietary habits of a lifetime is not easy. A half-hearted treatment will accomplish nothing more than postponing the inevitable, while strict adherence to the regimen in the early stages of the disease can reverse it. There are three fundamental steps: 1- It is necessary to decrease the total consumption of starches and sugars in order to reduce the need for insulin to levels that the pancreas can provide. That is to say that we are going to give the pancreas a vacation. Look at the table, the foods on the green list are very low in carbohydrates. These are the foods that one can consume in unlimited quantity without raising the level of glucose in the blood. Note that meals on the red list have more than 50 times the amount of carbohydrate for each 100g serving compared to foods on the green part of the list. Even the consumption of very small quantities of foods that appear on the red portion of the list completely sabotages the diet and guarantees failure. It is important to understand that one does NOT ask the patient to eat less, but only to avoid wheat, juice and bananas. Remember that junk food is high in starches, mainly wheat. If anything, you want your patient to eat more food, so that he does not feel hungry, but principally the foods on the green list. 2 - Daily physical activity should be increased consistently to increase the basal metabolic rate. For example, walk every day for an hour. Note that extreme sporadic exercise only burns an insignificant amount of calories. It is more important that exercise is daily or several times a day to lower glucose (and insulin levels). One has to increase the proportion of muscle mass compared to adipose tissue in order to achieve a higher basal metabolic rate and thus burn more calories. This can only be achieved when physical activity is engaged in consistently. 3- For most people it is necessary to reduce at least 10 to 15% of body weight in order to put diabetes into remission. Note that generally when one completely excludes juices and sweetened drinks, banana and wheat in all its forms (flour, cookies, bread, noodles, etc.) the weight loss is immediate. For most people you do not have to ask patients to eat less food ... simply insist that they eat vegetables, fish, turkey and eggs but NO sweetened beverages or bread and other flour products. When one consumes less than 20 grams of carbohydrates in a meal, the catabolism of fatty acids, known as ketosis begins. In the beginning, beans and fruits (except lemon juice) are omitted so that it is easier to achieve this goal of less than 20 grams of carbohydrate. Once, the weight loss has been achieved, modest amounts of beans can be eaten as well as fruits that are not bananas. Eating more than 20 grams of carbohydrate at one time is more than enough to stop the catabolism of fatty acids and eliminate the weight loss that is necessary for a long-lasting cure. As it is about burning fat, remember that the process of metabolizing fat produces ketosis, and in the first few days a person may feel a bit of nausea and should drink enough water for the acetone to come out in the urine. Weight loss is essential so that the disease does not return, but it must be easy if the diet is rigorously followed.
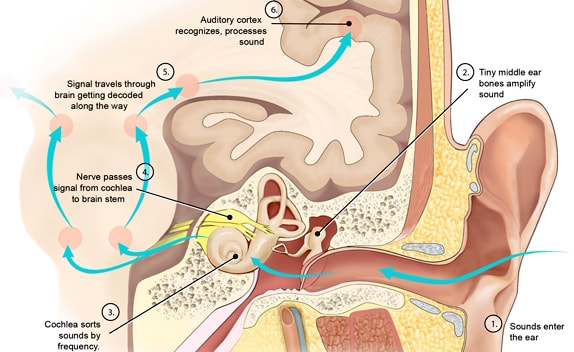
4- It is necessary to have objective evidence of progress. For example, the diabetic or pre-diabetic should weigh themselves regularly, if possible every day, to see how they are progressing in terms of the goal of weight loss to achieve a body mass index of 25. Post- prandial glucose should be measured with fingerstick glucometry 90 minutes after meals so that the patient can verify which are the foods that most raise the glucose level. Generally post-prandial glucose peaks should be routinely measured 90 minutes after meals with a glucometer. The goal is to verify that the glucose after eating food is below 140 mg/dL. If there is no consumption of wheat and flour, juices and sweetened drinks or bananas, it is likely that the glucose level will be acceptable.. Medications for diabetes are more appropriate for people who refuse to make dietary modifications. Even tiny amounts of bread will derail dietary efforts completely due to the Amylopectin A content in wheat. When it comes to wheat one should not instruct people to eat "just a little bit". If you add the carbohydrates of the foods in the table you will notice that a piece of bread or a cookie has more carbohydrates than a whole day of chicken, fish, eggs and turkey. By drastically reducing starch intake, glucose and triglyceride levels will drop, in addition to weight. Why not just take insulin instead instead of changing diet? For persons who still produce adequate quantities of insulin, adding additional exogenous insulin carries significant health risks. Excess insulin increases obesity, increases cancer risk and worsens hypertension through increased sodium reabsorption in the kidney. The use of endogenous insulin should be confined to individuals with hyperglycemia who have type 1 diabetes, who are significantly underweight, or who have medical emergencies. When does the diet not work? It is important to understand that no diet can be effective if one is taking steroid medications, since glucocorticoid medications (prednisone, prednisolone, dexamethasone, betamethasone etc) increase levels of serum glucose. Hydrochlorthiazide diuretics may also raise serum glucose slightly. It is also important to understand that during the process of lypolysis one of the byproducts is LDL cholesterol. A marked elevation of LDL cholesterol from one's own fat is transient and always occurs during periods of fasting or weight loss. When the weight stabilizes, the LDL cholesterol level stabilizes at normal levels. |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
August 2018
Categories |




 RSS Feed
RSS Feed