|
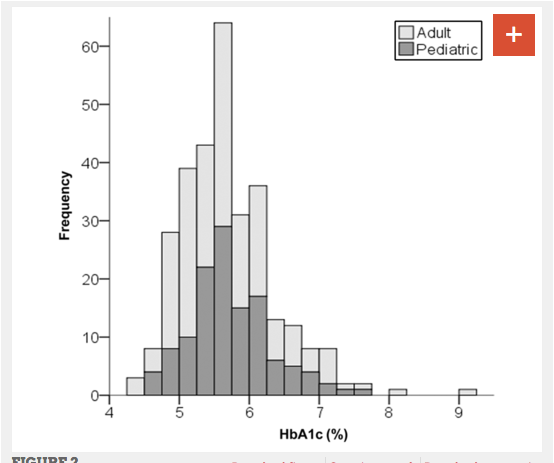
An observational study of 316 adults and children with type 1 diabetes published in the journal Pediatrics found that patients who followed a very low carbohydrate diet had exceptional glucose control. The duration of diabetes among participants in the study was an average of 11 years, and the average participant had followed a very low carbohydrate diet for 2.2 years. The mean daily carbohydrate intake was 36 grams per day. The mean HbA1c level was found to be 5.7% Only 7 participants (2%) had been hospitalized in the preceding year, of whom 4 (1%) had ketoacidosis and 2 (<1%) for hypoglycemia. The authors conclude that there is evidence that unusually good glucose control may be possible in type 1 diabetics using low-carbohydrate diets. Since the participants were all chosen on the basis of their low carbohydrate diet, this may represent a highly motivated subset of type 1 diabetics. Still it provides a basis to justify prospective randomized case control studies to verify this finding. Management of Type 1 Diabetes With a Very Low–Carbohydrate Diet
Belinda S. Lennerz, Anna Barton, Richard K. Bernstein, R. David Dikeman, Carrie Diulus, Sarah Hallberg, Erinn T. Rhodes, Cara B. Ebbeling, Eric C. Westman, William S. Yancy, David S. Ludwig Pediatrics May 2018, e20173349; DOI: 10.1542/peds.2017-3349
1 Comment
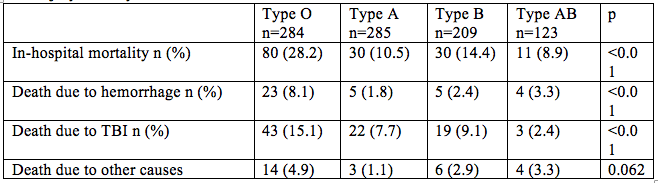
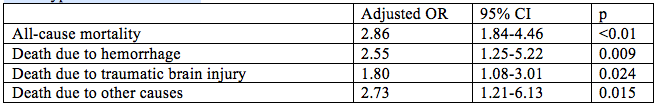
Trauma patients with type O are more likely to die from hemorrhage than other blood types according to researchers from the Tokyo Medical and Dental University. This retrospective observational study published in Critical Care included 901 trauma patients with injury severity scores >15. The adjusted odds ratio for death for persons with type O blood when compared with all other blood types were as follows: These findings indicate increased all-cause mortality, increased risk of death due to hemorrhage and to death due to traumatic brain injury among trauma victims with blood type O when compared to other blood types.[1] These findings are in keeping with previously published studies which have found that persons with type O blood have decreased risk of deep venous thrombosis [2] and increased risk of GI hemorrhage [3], obstetrical hemorrhage [4], and bleeding associated with anticoagulant usage [5] when compared to other blood types. The study investigators propose that this discrepancy may be due to decreased von Willebrand factor levels in persons with blood type O. [1] Takayama W, Endo A, Koguchi H, et al. The impact of blood type O on mortality of severe trauma patients: a retrospective observational study. Critical Care (2018) 22:100
[2] Spiezia L, Campello E, Bon M, et al. ABO blood groups and the risk of venous thrombosis in patients with inherited thrombophilia. Blood Transfusion. 2013;11(2):250-253. doi:10.2450/2012.0060-12. [3] Dentali F, Sironi AP, Ageno W, Bonfanti C, Crestani S, Frattini F, et al. Relationship between ABO blood group and hemorrhage: a systemic literature review and meta-analysis. Semin Thromb Hemost. 2013;39:72–82. [4]Drukker L, Srebnik N, Elstein D, et al. The association between ABO blood group and obstetric hemorrhage. J Thromb Thrombolytics 2016 Oct; 42(3):340-5. doi: 10.1007/s11239-016-1360-5. [5] Garcia AA, Van der Heijden JF, Meijers JCM, et al. The relationship between ABO blood group and the risk of bleeding during Vitamin K antagonist treatment. Journal of Thrombosis and Haemostasis, 4: 1418-1420. doi:10.1111/j.1538-7836.2006.01962.x A retrospective cohort study published in JAMA Internal Medicine looked at the hospital and primary care records of 46,634 patients for whom 20 years of blood pressure measurements were available. This investigation demonstrated that among the very elderly blood pressure peaks 14 to 18 years before death and then declines gradually. Among patients over the age of 90, the mean blood pressure drop is -22 mmHg and the decrease becomes linear between 3 and 10 years before death. The implication of these studies is that those who die of “old age” experience a gradual and predictable blood pressure decline. [1] An additional study published in JAMA Neurology performed autopsies on 303 persons who died with a mean of 87.2 years of age. Among the 297 who had blood pressure measurements 15.8% had chronic microinfarcts, 63.8% had cortical microinfarcts, 40.4% had subcortical microinfarcts, and 8.5% had infratentorial microinfarcts. Patients with and without infarcts had similar baseline systolic and diastolic blood pressures, but those with subcortical microinfarcts had a greater annual decline in blood pressure. [2] The tentative conclusion which can be drawn from these studies is that among the very old blood pressure in the range of 120 to 140 mmHg systolic may be beneficial for the maintenance of cerebral perfusion and avoidance of cognitive decline. Use of medications to control blood pressure among patients over the age of 85 should be examined closely to determine need, and where need is uncertain patients should be gradually tapered down under close medical supervision.
|
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
August 2018
Categories |



 RSS Feed
RSS Feed