|
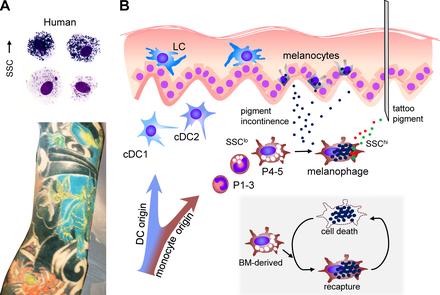
Today we are going to talk about a lifelong inflammatory process and some of the implications of this inflammatory process for disease. The pathologies we will talk about is the chronic inflammatory response to tattoos. In a recent article published in March 2018 in the Journal of Experimental Medicine titled "Unveiling skin macrophage dynamics explains both tattoo persistence and strenuous removal" Baranska et al explain what happens to tattoo ink when it is injected into the dermis. The pigment injected into the dermis generates an inflammatory response. A specific type of macrophage, known as a melanophage, along with other immune cells, race to engulf the foreign substance, in this case tattoo ink. In other words the ink does not stay in the dermis it is retained inside these macrophages. When the melanophage dies it then bursts, and then another melanophage engulfs the pigment which has been released. The result is an endless cycle of immune response and cell death of macrophages. While some of the pigment laden immune cells stay at the site where the tattoo was placed, others are taken by immune cells to the lymph nodes scattered throughout the body. Thus when you look at a tattoo, you are actually looking at a collection of dying macrophages in the skin. Every 90 days these macrophages die and are replaced by new macrophages. Tattoo associated diseases In order to read the most recent research related to tattoo related diseases click on the links below::
Bacterial endocarditis, aortic regurgitation, and heart failure https://heart.bmj.com/content/85/1/11 https://www.ncbi.nlm.nih.gov/pubmed/18710675 https://www.sciencedirect.com/science/article/pii/S0167527307018761 https://link.springer.com/article/10.1007/s00059-013-3810-6 Systemic sarcoidosis and granulomas https://www.nejm.org/doi/full/10.1056/nejmicm1215331 https://www.sciencedirect.com/science/article/pii/S0926995998001238 Uveitis https://www.nature.com/articles/eye201017 https://onlinelibrary.wiley.com/doi/full/10.1111/aos.12216 https://www.aao.org/editors-choice/seven-cases-of-tattooassociated-uveitis Non-tuberculous mycobacteria https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6133a3.htm https://www.ncbi.nlm.nih.gov/pubmed/23704119 https://www.medscape.com/viewarticle/771466_transcript https://www.medpagetoday.com/infectiousdisease/generalinfectiousdisease/27993 Inflammatory myopathy and immune deficiency https://www.mdedge.com/edermatologynews/article/168368/mixed-topics/inflammatory-myopathy-following-tattoo-reported https://www.techtimes.com/articles/230653/20180620/woman-suffers-3-years-of-chronic-pain-after-getting-tattoo-heres-what-happened.htm Haemophilus influenza sepsis https://www.consultant360.com/articles/rare-tattoo-complication-haemophilus-influenzae-sepsis-teenager Hepatitis C https://aasldpubs.onlinelibrary.wiley.com/doi/pdf/10.1002/hep.26245 https://www.sciencedirect.com/science/article/pii/S1201971210024227 https://www.ncbi.nlm.nih.gov/pubmed/23315899 Painful pigmented lymphadenopathy which mimics melanoma, lymphoma or breast cancer https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1325237/ https://www.ajemjournal.com/article/S0735-6757(13)00113-7/abstract https://www.ncbi.nlm.nih.gov/pubmed/8556264 Pyoderma gangrenosum https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4150710/ https://www.jaad.org/article/S0190-9622(15)00445-4/abstract?code=ymjd-site Psoriasis, discoid lupus erythematosus and lichen planus https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4391350/ https://jamanetwork.com/journals/jamadermatology/article-abstract/522265 https://onlinelibrary.wiley.com/doi/abs/10.1002/art.21334 http://www.cmaj.ca/content/185/7/585 Malignant melanoma, basal cell carcinoma, squamous cell carcinoma, dermatofibrosarcoma protuberans, B cell lymphoma and leiomyosarcoma. https://www.ncbi.nlm.nih.gov/pubmed/21818504 https://www.ncbi.nlm.nih.gov/pubmed/18521416 https://www.jprasurg.com/article/0007-1226(83)90103-0/pdf Infection, Allergic Contact Dermatitis and Keloids http://www.cmaj.ca/content/185/7/585 Thousands of adverse effects have been reported in medical journals around the world including India https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3519250/ Denmark https://www.karger.com/Article/FullText/452148 Finland https://www.karger.com/Article/FullText/468536 Here is a book dedicated to complications of tattoos https://books.google.com/books?id=r1diDwAAQBAJ&pg=PA85&lpg=PA85&dq=discoid+lupus+erythematosus+tattoos&source=bl&ots=Rql_-b5BUb&sig=eXeVVYkBhWqAon-GqHQSoDAYQZs&hl=en&sa=X&ved=2ahUKEwjkvP_S1IndAhXIqVQKHfpHBTs4FBDoATAHegQIARAB#v=onepage&q=discoid%20lupus%20erythematosus%20tattoos&f=false
0 Comments
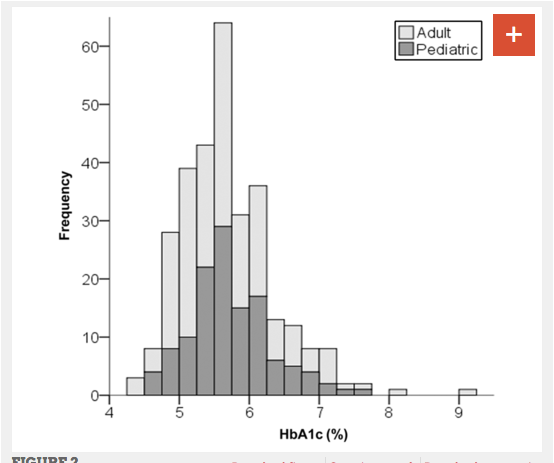
An observational study of 316 adults and children with type 1 diabetes published in the journal Pediatrics found that patients who followed a very low carbohydrate diet had exceptional glucose control. The duration of diabetes among participants in the study was an average of 11 years, and the average participant had followed a very low carbohydrate diet for 2.2 years. The mean daily carbohydrate intake was 36 grams per day. The mean HbA1c level was found to be 5.7% Only 7 participants (2%) had been hospitalized in the preceding year, of whom 4 (1%) had ketoacidosis and 2 (<1%) for hypoglycemia. The authors conclude that there is evidence that unusually good glucose control may be possible in type 1 diabetics using low-carbohydrate diets. Since the participants were all chosen on the basis of their low carbohydrate diet, this may represent a highly motivated subset of type 1 diabetics. Still it provides a basis to justify prospective randomized case control studies to verify this finding. Management of Type 1 Diabetes With a Very Low–Carbohydrate Diet
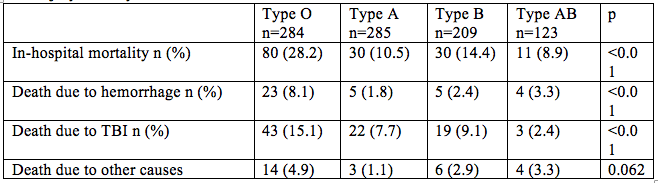
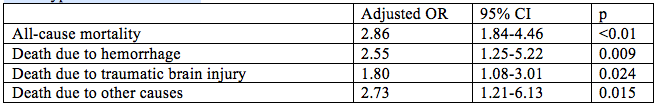
Belinda S. Lennerz, Anna Barton, Richard K. Bernstein, R. David Dikeman, Carrie Diulus, Sarah Hallberg, Erinn T. Rhodes, Cara B. Ebbeling, Eric C. Westman, William S. Yancy, David S. Ludwig Pediatrics May 2018, e20173349; DOI: 10.1542/peds.2017-3349 Trauma patients with type O are more likely to die from hemorrhage than other blood types according to researchers from the Tokyo Medical and Dental University. This retrospective observational study published in Critical Care included 901 trauma patients with injury severity scores >15. The adjusted odds ratio for death for persons with type O blood when compared with all other blood types were as follows: These findings indicate increased all-cause mortality, increased risk of death due to hemorrhage and to death due to traumatic brain injury among trauma victims with blood type O when compared to other blood types.[1] These findings are in keeping with previously published studies which have found that persons with type O blood have decreased risk of deep venous thrombosis [2] and increased risk of GI hemorrhage [3], obstetrical hemorrhage [4], and bleeding associated with anticoagulant usage [5] when compared to other blood types. The study investigators propose that this discrepancy may be due to decreased von Willebrand factor levels in persons with blood type O. [1] Takayama W, Endo A, Koguchi H, et al. The impact of blood type O on mortality of severe trauma patients: a retrospective observational study. Critical Care (2018) 22:100
[2] Spiezia L, Campello E, Bon M, et al. ABO blood groups and the risk of venous thrombosis in patients with inherited thrombophilia. Blood Transfusion. 2013;11(2):250-253. doi:10.2450/2012.0060-12. [3] Dentali F, Sironi AP, Ageno W, Bonfanti C, Crestani S, Frattini F, et al. Relationship between ABO blood group and hemorrhage: a systemic literature review and meta-analysis. Semin Thromb Hemost. 2013;39:72–82. [4]Drukker L, Srebnik N, Elstein D, et al. The association between ABO blood group and obstetric hemorrhage. J Thromb Thrombolytics 2016 Oct; 42(3):340-5. doi: 10.1007/s11239-016-1360-5. [5] Garcia AA, Van der Heijden JF, Meijers JCM, et al. The relationship between ABO blood group and the risk of bleeding during Vitamin K antagonist treatment. Journal of Thrombosis and Haemostasis, 4: 1418-1420. doi:10.1111/j.1538-7836.2006.01962.x A retrospective cohort study published in JAMA Internal Medicine looked at the hospital and primary care records of 46,634 patients for whom 20 years of blood pressure measurements were available. This investigation demonstrated that among the very elderly blood pressure peaks 14 to 18 years before death and then declines gradually. Among patients over the age of 90, the mean blood pressure drop is -22 mmHg and the decrease becomes linear between 3 and 10 years before death. The implication of these studies is that those who die of “old age” experience a gradual and predictable blood pressure decline. [1] An additional study published in JAMA Neurology performed autopsies on 303 persons who died with a mean of 87.2 years of age. Among the 297 who had blood pressure measurements 15.8% had chronic microinfarcts, 63.8% had cortical microinfarcts, 40.4% had subcortical microinfarcts, and 8.5% had infratentorial microinfarcts. Patients with and without infarcts had similar baseline systolic and diastolic blood pressures, but those with subcortical microinfarcts had a greater annual decline in blood pressure. [2] The tentative conclusion which can be drawn from these studies is that among the very old blood pressure in the range of 120 to 140 mmHg systolic may be beneficial for the maintenance of cerebral perfusion and avoidance of cognitive decline. Use of medications to control blood pressure among patients over the age of 85 should be examined closely to determine need, and where need is uncertain patients should be gradually tapered down under close medical supervision.
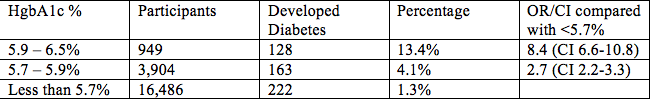
A recent investigation found that the HgbA1c test is a more reliable screening tool for diabetes risk than a fasting glucose. Persons enrolled in the study all had normal fasting glucose levels less than 100 mg/dl and Hgb A1c < 6.5 %, and therefore were considered low risk for diabetes.
The persons who had an HgbA1c between 5.9 and 6.5 were more than 8 times more likely to develop diabetes within 4 years than a person with a normal fasting glucose and a HgbA1c less than 5.7% A study of 35 middle-aged adults conducted by UCLA researchers showed that those participants who spend more time sitting have the medial temporal lobe thickness, that is, an increase in brain atrophy compared with people who do spend much time seated.
Temporary medial atrophy detected by magnetic resonance is a finding which is found in cases of memory loss and Alzheimer's disease. Siddarth P, Burggren AC, Eyre HA et al. Sedentary behavior associated with reduced medial temporal lobe thickness in middle-aged and older adults. PLoS ONE 13 (4): e0195549. https://doi.org/10.1371/journal.pone.0195549 Researchers at the University of California San Diego and Seoul National University report that person with 25-hydroxyvitamin D levels below 30 ng/ml have a 5 times greater risk for developing type 2 diabetes than people with levels above 50 ng/ml.
The prospective cohort study enrolled 904 healthy adults with a mean age of 74 years and followed them for 10 to 12 years. During that time 337 patients developed pre-diabetes and 47 patients developed diabetes. Persons with 25-hydroxyvitamin D levels > 50 ng/ml had an HR = 0.19, CI = 0.06–0.56 when compared to individuals with 25 hydroxyvitamin D levels < 30 ng/ml. This means that individuals with higher 25-hydroxyvitamin D levels had an 81% decreased probability of developing prediabetes or diabetes. Multiple recent research studies have found strong correlations between low levels of vitamin D and depression , dementia, schizophrenia, type 2 diabetes, and hypertension yet supplementation with pharmacologic vitamin D has not been proven to be as beneficial as outdoor activities to raise vitamin D levels. There is a real possibility that sedentary behavior and lack of exercise is the confounding factor in this correlation between vitamin D and diabetes. After all lack of exercise leads to increased glucose, increased adiposity, hypertension, hyperglycemia and for many people decreased exposure to the sunshine which is necessary for vitamin D formation. One of the recurrent nightmares faced by emergency medicine physicians is: What to do with a severely depressed and suicidal patient when there are no beds in a psychiatric facility? Recent studies have indicated that one option may be ketamine. Previous studies of injected ketamine had indicated some benefits, but raised real concerns about the need for vital signs monitoring and prolonged observation prior to discharge. This new study published in the American Journal of Psychiatry shows significant improvement in suicidal ideation and depression after administration of ketamine vía nasal aerosol. In a double blind, multi-center prospective study, 68 people with severe depression or suicidal ideation were randomly assigned to receive 84 mg of intranasal ketamine or placebo twice weekly for 4 weeks. Significant improvement of depression was observed at 4 hours and at 24 hours in the group which received ketamine. Ketamine also improved suicidal ideation at 4 hours, although not at 24 hours. Ketamine is not innocuous. Adolescents in particular may experience a adverse reaction where they become transiently agitated. Someone experienced with the use of ketamine should be present. While certainly this is far from definitive treatment, it possibly provides an additional treatment option for emergency situations. Canuso CM, Singh JB. Fedgchin M, Alphs L et al. Efficacy and Safety of Intranasal Esketamine for the Rapid Reduction of Symptoms of Depression and Suicidality in Patients at Imminent Risk for Suicide: Results of a Double-Blind, Randomized, Placebo-Controlled Study. American Journal of Psychiatry 2018
juices and sweetened beverages associated with increased mortality from coronary vascular disease.4/16/2018 Researchers have reported that increased consumption of juices and sweetened beverages is associated with cardiovascular disease and increased mortality among the overweight. The REGARDS study involved 17,930 participants age 45 years and older who were followed for an average of 6,9 years. There were 1465 deaths of whom 279 were associated with coronary artery disease. Those who drink more sweetened beverages and fruit juices doubled their risk of death from coronary vascular disease compared to those who consumed the least amount. This effect was strongest among obese patients. [1]
These results were reported in the American Heart Association's Epidemiology and Prevention Scientific Sessions 2018. Over the mean follow-up period of 6.9 years, there were a total of 1465 all-cause deaths and 279 coronary heart disease deaths among the 17,930 participants. The risk of coronary vascular disease was highest among those who consumed a mean of 20 ounces of juices and sweetened beverages. (Hazard ratio [HR], 2.0; 95% CI, 1.12 - 3.54) compared with those who consumed a mean of 0.8 ounces. Persons with a BMI between 25 and 29,9 also had increased mortality associated with increased juice and sweetened beverage consumption (HR, 1.12; 95% CI, 1.02 - 1.22; P = .04), There are many explanations for this phenomenon. Increased sweetened beverage and juice consumption leads to increased insulin stimulation (due to glucose), increased hepatic gluconeogenesis, advanced glycation end products, and increased triglyceride levels (due to fructose and glucose) all of which contribute to formation of oxidized LDL, atherosclerosis and heart failure. [2] [1] Collin L, Safford M, Vaccarino V and Welsh J. Abstract P235: Sugar-Sweetened Beverage and Food Intake and Mortality Risk Among U.S. Adults Circulation, 2018;137:AP235, originally published March 21, 2018 http://circ.ahajournals.org/content/137/Suppl_1/AP235 [2] Basta G, Schmidt AM, De Caterina R; Advanced glycation end products and vascular inflammation: implications for accelerated atherosclerosis in diabetes, Cardiovascular Research, Volume 63, Issue 4, 1 September 2004, Pages 582–592 https://academic.oup.com/cardiovascres/article/63/4/582/318389 In a cross sectional study published in the Journal of the American Heart Association looking at 4,426 participants with a median age of 50 years in Sao Paolo Brazil, researchers found that consumption of > 3 cups of coffee per day by persons who have never smoked led to a 63% decrease in the odds of finding significant coronary artery calcifications by CT scan. (OR: 0.37 [95% confidence interval, 0.15–0.91])
Miranda AM, Steluti J, Goulart AC et al. Consumption and Coronary Artery Calcium Score: Cross‐Sectional Results of ELSA‐Brasil (Brazilian Longitudinal Study of Adult Health) Journal of the American Heart Association. 2018;7:e007155, originally published March 24, 2018 |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
August 2018
Categories |










 RSS Feed
RSS Feed